Prescriptions and Medication
Ordering repeat prescriptions
The easiest ways to order repeat prescriptions are:
- using your NHS account (through the NHS website or in the NHS App)
These accounts show you all your repeat medicine and dosage and you can choose the ones you need.
You can also:
- bring the paper form to the surgery, Monday to Friday between 8am-6.30pm
We do not take repeat prescription requests over the phone or email.
Collecting your prescription
We aim to process all repeat prescription requests within 3 working days of receipt. You will need to check with your pharmacy how long their turnaround time for prescriptions is - this can be upto 14 days in some instances.
You will need to choose a pharmacy to collect your prescription from. We call this nominating a pharmacy.
You can change your nominated pharmacy at any time:
- on the app or website where you order repeat prescriptions
- at your GP practice
- at any pharmacy that accepts repeat prescriptions
Electronic prescription service
The Electronic Prescription Service (EPS) is an NHS service. It gives you the chance to change how your GP sends your prescription to the place you choose to get your medicines or appliances from.
What does this mean for you?
You will have more choice about where to get your medicines from because they can be collected from a pharmacy near to where you live, work or shop.
For further information on:
- Choosing a pharmacy or other dispenser
- Cancelling or changing your choice of pharmacist or dispenser
- What can I do if I'm unhappy with the process?
Questions about your prescription
If you have questions about your medicine, your local pharmacists can answer these. They can also answer questions on medicines you can buy without a prescription.
If you are phoning regarding the status of your presciption please check your app if you have this facility or with your pharmacy first
The NHS website has information on how your medicine works, how and when to take it, possible side effects and answers to your common questions.
If you would like to speak to someone at the GP surgery about your prescription:
- Prescription queries are dealt with between the hours of 9am and 1pm. We do NOT have a voicemail facility. If your call is urgent please press option 1 outside of these times.
- Please check your app if you have this facility or with your pharmacy if your prescription has been sent
- fill in our medication query form.
Medication reviews
If you have a repeat prescription, we may ask you to come in for a regular review. We will be in touch when you need to come in for a review.
Prescription charges
Find out more about prescription charges (nhs.uk).
What to do with old medicines
Take it to the pharmacy you got it from or bring it in to the surgery. Do not put it in your household bin or flush it down the toilet.
Counterfeit versus falsified medicines
Counterfeit medicines are fake medicines that are often produced in unsafe and unsanitary conditions. This means they are not inspected by regulatory authorities, making it impossible to know what ingredients the counterfeit medicines contain.
Counterfeits can be very dangerous and are a serious public health risk. The primary danger in taking a counterfeit medicine is that patients are putting something into their body that may not help their current condition and, more alarmingly, could result in harmful effects to their overall health.
Experts have identified harmful substances within counterfeit medicines such as boric acid, leaded highway paint, floor polish, brick dust and heavy metals.
Falsified medicines are fake medicines that pass themselves off as real, authorised medicines. The European Union (EU) has a strong legal framework for the licensing, manufacturing, and distribution of medicines, centred around the Directive on falsified medicines for human use, so that only licensed pharmacies and approved retailers are allowed to offer medicines for sale, including legitimate sale via the internet. The European Medicines Agency works closely with its partners on the implementation of these laws.
Falsified medicines may:
- contain ingredients of low quality or in the wrong doses.
- be deliberately and fraudulently mislabelled with respect to their identity or source.
- have fake packaging, the wrong ingredients, or low levels of the active ingredients.
Falsified medicines do not pass through the usual evaluation of quality, safety and efficacy that is required for the EU authorisation procedure. Because of this, they can be a health threat.
Until recently, the most frequently falsified medicines in wealthy countries were expensive lifestyle medicines, such as hormones, steroids, and antihistamines. In developing countries, they have included medicines used to treat life-threatening conditions such as malaria, tuberculosis, and HIV / AIDS.
In June 2024, The World Health Organisation (WHO) issued a medical product alert on falsified semaglutides (medicines that are used for treatment of type 2 diabetes and obesity). The alert addressed 3 falsified batches of product of specific brand Ozempic which had been detected in Brazil, the United Kingdom and the United States of America. Details of the alert can be found at WHO issues warning on falsified medicines used for diabetes treatment and weight loss.
The phenomenon of falsified medicines is on the increase, with more and more medicines now being falsified. These include expensive medicines, such as anticancer medicines, and medicines in high demand, such as antivirals.
Falsified vs. counterfeit medicines.
Falsified medicines are not the same as counterfeit medicines:
- Falsified medicinesare fake medicines that are designed to mimic real medicines.
- Counterfeit medicinesare medicines that do not comply with intellectual-property rights or that infringe trademark law.
Medicines on the internet
Obtaining medicines through unregulated and unregistered internet sites or via social media poses a potentially serious health risk, as these medicines are not made by trained scientists under the rigorous conditions required for patient safety.
Patients also increase their risk of being victims of credit card fraud or having their identities stolen.
Prescription medicines should only be used as prescribed by, and under the supervision of, a qualified healthcare professional. When purchasing medicines online, patients should be mindful to only choose a pharmacy or online retailer that is registered with the MHRA or Royal Pharmaceutical Society of Great Britain
All pharmacies operating in Great Britain must be registered with The General Pharmaceutical Council (GPhC), who also operate a voluntary internet pharmacy logo scheme. The logo helps consumers to identify legitimate online pharmacies so that you can be sure you are purchasing safe and genuine medicines online. The GPhC logo contains the pharmacy’s unique seven-digit registration number, and when clicked takes the user to the Royal Pharmaceutical Society of Great Britain (RPSGB) website to help verify the pharmacy.
The Medicines and Healthcare products Regulatory Agency (MHRA), run the #FakeMeds campaign, which helps to protect patients’ health and money by providing quick and easy tools so they can avoid fake medical products when they shop online.
Useful links
https://fakemeds.campaign.gov.uk
https://fakemeds.campaign.gov.uk/wp-content/uploads/sites/13/2020/03/FakeMeds-toptips-General-2020.pdf?utm_source=FakeMeds-web&utm_medium=website&utm_campaign=COVID-19
Sick day rules
Medicine sick day guidance
Taking certain medicines when you are dehydrated or very unwell can result in you developing a more serious illness. This is because they can increase the risk of dehydration and lead to potentially serious side effects. This is known as Medicine Sick Day Rules. These medicines should be temporarily stopped if you are at risk of becoming dehydrated with any of the following:
- Vomiting or diarrhoea (unless only minor)
- Fevers, sweats or shaking
You can restart the medication after 24 to 48 hours of eating and drinking normally. Do not take extra for missed doses.
Which medications should I stop?
- ACE inhibitors: names ending in ‘pril’ - examples: lisinopril, perindopril, ramipril. A medicine for high blood pressure and heart conditions. If you are dehydrated, these medicines can stop your kidneys working properly.
- ARBs: names ending in ‘sartan’ - examples: losartan, candesartan, valsartan. A medicine for high blood pressure and heart conditions. If you are dehydrated, these medicines can stop your kidneys working properly.
- Diuretics: sometimes called ‘water pills’ - examples: furosemide, bendroflumethiazide, indapamide, spironolactone. Used for excess fluid and high blood pressure. These medicines can make dehydration more likely.
- NSAIDs: anti-inflammatory pain killers - examples: ibuprofen, naproxen, diclofenac. If you are dehydrated, these medicines can stop your kidneys working properly.
- Metformin: a medicine for diabetes. Dehydration can make it more likely that you will develop a serious side effect called lactic acidosis.
- SGLT2 inhibitors: names ending in ‘flozin’ - examples: canagliflozin, dapagliflozin, empagliflozin, ertugliflozin. A medication used in the treatment of Diabetes, Kidney disease or Heart Failure. These medicines can make dehydration more likely and if you have diabetes can cause acid to build up if you are unwell.
More information relating to SGLT2 inhibitors
Which illnesses cause dehydration?
Dehydration is the loss of fluid from your body. Vomiting, diarrhoea, and fever (high temperature, sweats, shaking) can make you dehydrated. If you are sick once or have diarrhoea once, then you are unlikely to become dehydrated. Having two or more episodes of vomiting or diarrhoea can lead to dehydration: in these cases, you should consider following this advice.
What actions should I take?
If you develop a dehydrating illness, you should temporarily stop taking any medicine listed here, and any other medicine identified by your health professional. It is very important that you restart your medicine once you have recovered from the illness. This would normally be after 24 to 48 hours of eating and drinking normally. When you restart your medicine, just take them as normal. Do not take extra for the doses you have missed
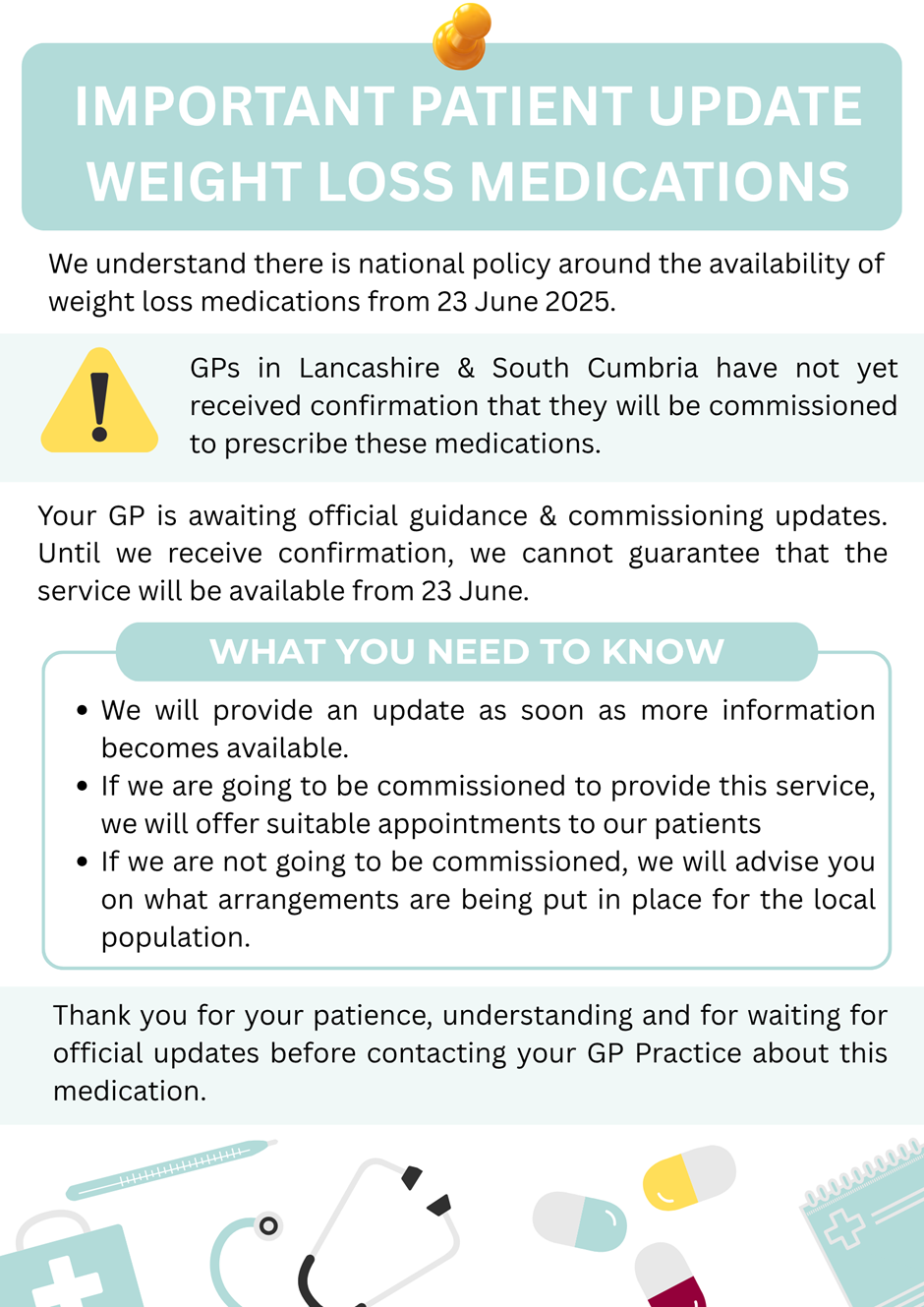
WEIGHT LOSS MEDICATION
Page created: 06 September 2024